Overview
Gastritis refers to inflammation, irritation, or erosion of the stomach lining. This condition can occur suddenly (acute gastritis) or develop gradually over time (chronic gastritis). Symptoms of gastritis can include:
- Abdominal pain or discomfort
- Nausea and vomiting
- Indigestion or heartburn
- Loss of appetite
- Bloating or feeling of fullness
- Belching
- Dark or black stools
- Vomiting blood
Gastritis can be caused by various factors, including:
- Helicobacter pylori infection (H.pylori): This bacteria is a common cause of gastritis and can lead to inflammation and damage to the stomach lining. People infected with H. pylori are at increased risk of developing gastritis and other gastrointestinal conditions
- NSAIDS-Regular use of NSAIDs: such as aspirin, ibuprofen, or naproxen, can irritate the stomach lining and contribute to the development of gastritis. Long-term use of NSAIDs, especially at high doses, is associated with an elevated risk of gastritis and peptic ulcers
- Excessive alcohol consumption: Alcohol can irritate the stomach lining, leading to inflammation and gastritis. Excessive alcohol consumption can irritate the stomach lining and predispose individuals to gastritis.
- Autoimmune diseases: Conditions such as autoimmune gastritis, where the body’s immune system mistakenly attacks the stomach lining, can cause chronic inflammation and damage.
How is it diagnosed?
You physician might recommend an upper endoscopy. This procedure allows the physician to look for inflammation, erosions, or other abnormalities. Biopsies may be taken to help confirm the diagnosis of gastritis and identify the underlying cause. Your physician might also order blood or stool tests to detect infections, anemia or inflammation.
How is it treated?
Gastritis can be treated in a variety of ways including:
- Proton Pump Inhibitios (PPI’s) and H2 receptor antagonists: These medications reduce stomach acid production, helping to alleviate symptoms and promote healing of the stomach lining.
- Lifestyle and Dietary Changes: Avoiding spicy, acidic, or irritating foods can help reduce inflammation and alleviate symptoms. Excessive alcohol and caffeine consumption can aggravate gastritis symptoms and delay healing. Limiting or avoiding these may help improve symptoms. Practicing relaxation techniques such as deep breathing, meditation, or yoga can help reduce stress levels, which may contribute to gastritis symptoms.
- Regular follow-up appointments: appointments with a healthcare provider are essential to monitor response to treatment, adjust medications if necessary, and address any ongoing symptoms or concerns.
References
Mayo Clinic. 2024. Gastritis. https://www.mayoclinic.org/diseases-conditions/gastritis/symptoms-causes/syc-20355807
Cleveland Clinic. 2023. Gastritis. https://my.clevelandclinic.org/health/diseases/10349-gastritis
Gastrointestinal Bleeding
Overview
Gastrointestinal bleeding refers to any bleeding that occurs in the digestive tract, from the mouth to the rectum. Upper GI bleeding involves the esophagus, stomach and duodenum (the first part of the small intestine). Lower GI bleeding involves the large intestine which includes the appendix, colon and rectum.
GI bleeding can vary depending on the location and severity of the bleeding.
- Bright red or maroon-colored blood in vomit or stool
- Black, tarry stools; which may indicate bleeding higher up in the digestive tract
- Abdominal pain or discomfort
- Weakness, dizziness, or lightheadedness
- Fatigue
- Shortness of breath
Causes of upper gastrointestinal bleeding can include peptic ulcers, esophagitis tears, esophageal varices, esophagitis and hiatal hernia. Causes of lower gastrointestinal bleeding can include inflammatory bowel disease, proctitis, diverticulitis, colon polyps, hemorrhoids, anal fissures and tumors.
How is it diagnosed?
A variety of tests may be ordered including
- Capsule Endoscopy: This procedure uses a capsule with a tiny camera in it to take pictures of the digestive tract. The capsule is swallowed like a pill and provides images of the small intestine, an area not usually reached on other endoscopy procedures. These pictures are sent to a recorder outside the body. The capsule passes out of the body through the stool within a few days. A capsule endoscopy is mostly used to check for problems within the small intestine which can include symptoms such as bleeding and varices
- Colonoscopy: This procedure involves inserting a flexible tube with a camera into the rectum to examine the large intestine. It can help identify sources of lower GI bleeding, such as colon polyps or tumors.
- EGD or upper endoscopy: An EGD uses a lighted, flexible endoscope to see inside the upper GI tract. The upper GI tract includes the esophagus, stomach, and duodenum—the first part of the small intestine. It allows for visualization of any bleeding spots, ulcers, or abnormalities.
- Imaging studies: Imaging tests such as CT scans, MRI scans, or angiography may be used to locate sources of bleeding or assess for complications such as arterial bleeding.
- Blood and stool tests: These tests check signs for blood loss like anemia and blood in the stool
How is it treated?
Most of the time, GI bleeding stops on its own. Medications like proton pump inhibitors (PPIs), H2-receptor antagonists, and antacids can be prescribed to reduce stomach acid production and promote healing of ulcers. Surgery might be needed in cases of severe or persistent bleeding that cannot be controlled with endoscopic or medical therapies.
References
Mayo Clinic. 2023. Gastrointestinal Bleeding. https://www.mayoclinic.org/diseases-conditions/gastrointestinal-bleeding/symptoms-causes/syc-20372729
Cleveland Clinic. 2022. Gastrointestinal Bleeding. https://my.clevelandclinic.org/health/diseases/23391-gastrointestinal-gi-bleeding
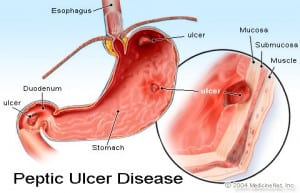
Peptic Ulcers
Overview
Peptic ulcers are commonly referred to as open sores that develop on the lining of the stomach, small intestine, or esophagus. They can be painful and lead to complications if left untreated. Peptic ulcers can develop due to various factors, including infection with Helicobacter pylori (H. pylori) bacteria, long-term use of NSAIDs, such as aspirin or ibuprofen, excessive alcohol consumption, smoking, and stress. Common symptoms of peptic ulcers may include abdominal pain or discomfort, bloating, belching, nausea, heartburn, and intolerance to fatty foods.
How is it diagnosed?
- EGD or upper endoscopy: An EGD uses a flexible endoscope to see inside the upper GI tract. The upper GI tract includes the esophagus, stomach, and duodenum—the first part of the small intestine. It can also be used to biopsy tissue in the upper GI tract to check for inflammation and ulcers, and determine the causes of abdominal pain, nausea, vomiting and anemia.
- Barium X-Ray: This imaging test involves drinking a liquid containing barium, which coats the lining of the digestive tract and makes ulcers more visible on X-rays.
How is it treated?
Treatment for peptic ulcers typically involves medications to reduce stomach acid production, antibiotics to eradicate H. pylori infection if present, and lifestyle modifications such as avoiding NSAIDs, alcohol, and smoking. Surgery may be necessary in severe cases or if complications like bleeding or perforation occur. Stress and spicy foods don’t cause ulcers but they can make your symptoms worse.
References
Mayo Clinic. 2022. Peptic Ulcer. https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc-20354223
Medline Plus. National Institutes of Health-National Library of Medicine. 2024. https://medlineplus.gov/pepticulcer.html#cat_92


